When choosing materials for surgical implants and medical devices, the debate between medical titanium plate and alloy-steel plate centers on biocompatibility, performance, and long-term safety. Medical titanium plates consistently outperform alloy-steel alternatives in critical areas including corrosion resistance, tissue compatibility, and strength-to-weight ratios. While alloy-steel plates may offer initial cost advantages, titanium's superior biocompatibility and reduced inflammatory response make it the preferred choice for permanent implants and critical surgical applications.

Understanding Medical Titanium Plates: The Gold Standard
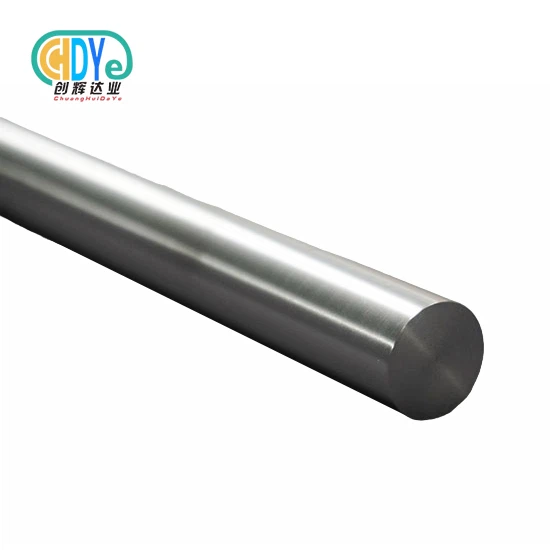
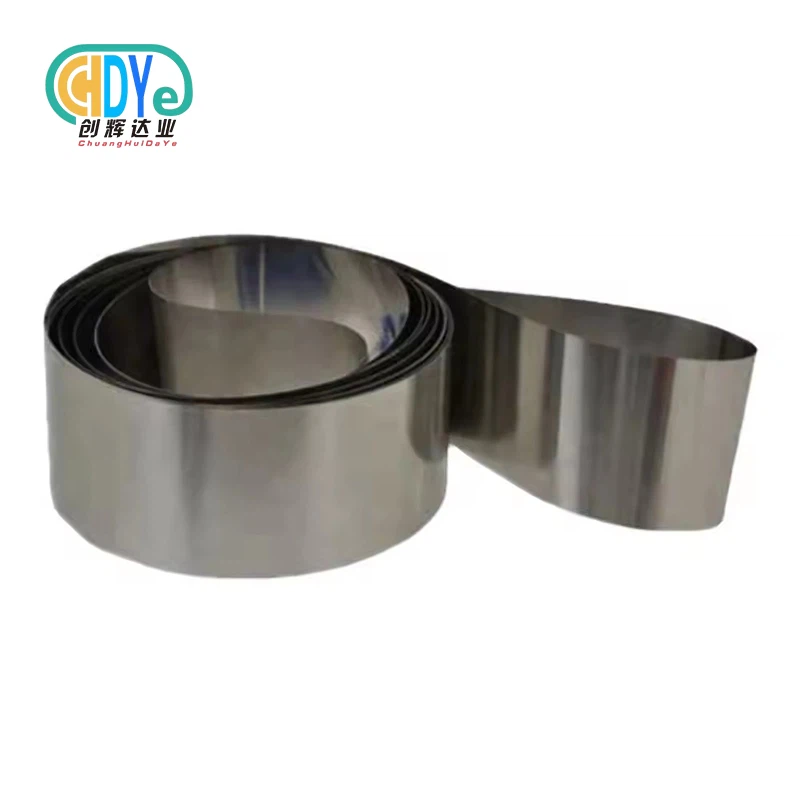
Medical titanium plates speak to precision-engineered arrangements outlined particularly for surgical applications. These biocompatible titanium components utilize high-purity titanium amalgams, especially Review 5 (Ti-6Al-4V) and Review 23 ELI (Additional Moo Interstitial), which convey uncommon execution in physiological environments.
The fabricating handle includes vacuum dissolving, controlled rolling, and exact warm treatment to accomplish ideal grain structure. This comes about in titanium bone plates that display surprising mechanical properties whereas keeping up idealize compatibility with human tissue.
Key characteristics include:
- Density of 4.5 g/cm³ compared to steel's 7.8 g/cm³
- Tensile quality extending from 895-1000 MPa
- Young's modulus of 110 GPa, closely coordinating bone
- Zero attractive impedances with therapeutic imaging
If you require lightweight inserts with prevalent biocompatibility, at that point orthopedic titanium plate arrangements are more reasonable than routine steel alternatives.
Alloy-Steel Plates in Medical Applications: Limited But Present
Alloy-steel plates, ordinarily 316L stainless steel, have generally served restorative applications due to their mechanical quality and beginning taken a toll viability. These materials contain chromium, nickel, and molybdenum increments that upgrade erosion resistance compared to carbon steel.
However, stainless steel's therapeutic applications confront critical limitations:
- Potential nickel particle discharge causing unfavorably susceptible reactions
- Higher flexible modulus making stress-shielding effects
- Magnetic properties interferometer with MRI procedures
- Inferior long-term erosion resistance in body fluids
Current restorative hone confines stainless steel basically to transitory obsession gadgets and outside surgical rebellious. The material's thickness of 7.9 g/cm³ makes pointless weight burden for patients requiring changeless implants.
If you require brief obsession arrangements with prompt accessibility, at that point medical-grade stainless steel may suffice for short-term applications.
Head-to-Head Performance Comparison
| Property | Medical Titanium Plate | Alloy-Steel Plate |
|---|---|---|
| Biocompatibility | Excellent (Class VI) | Good (316L grade) |
| Density (g/cm³) | 4.5 | 7.9 |
| Tensile Strength (MPa) | 895-1000 | 580-750 |
| Elastic Modulus (GPa) | 110 | 200 |
| MRI Compatibility | Non-magnetic | Magnetic interference |
| Corrosion Resistance | Superior | Moderate |
Laboratory testing reveals significant performance differences between these materials. Titanium alloy plate specimens demonstrate 40% better fatigue resistance under cyclic loading conditions typical of bone movement.
Electrochemical studies show titanium's passive oxide layer provides exceptional protection against body fluid corrosion, while stainless steel exhibits measurable ion release over extended periods.
Biocompatibility: The Critical Difference
Laboratory testing uncovers critical execution contrasts between these materials. Titanium combination plate examples illustrate 40% way better weakness resistance beneath cyclic stacking conditions normal of bone movement.
Electrochemical considers appear titanium's detached oxide layer gives remarkable assurance against body liquid erosion, whereas stainless steel shows quantifiable particle discharge over expanded periods.
Biocompatibility: The Basic Difference
Biocompatibility speaks to the most significant figure recognizing these materials. Restorative embed titanium accomplishes Course VI biocompatibility certification, demonstrating no poisonous, bothering, or provocative reaction in tissue contact applications.
Clinical ponders illustrate that biocompatible titanium advances osseointegration—the coordinate basic and utilitarian association between living bone and embed surface. This prepare happens inside 3-6 months post-surgery, making changeless tying down prevalent to any mechanical fixation.
Stainless steel needs this osseointegration capability. The fabric shapes sinewy tissue epitome or maybe than bone holding, possibly driving to embed releasing over time.
Three center biocompatibility points of interest of titanium:
- Zero allergenic potential compared to nickel-containing steels
- Stable oxide layer avoiding particle release
- Chemical inactivity keeping up tissue pH balance
If you require lasting inserts requiring tissue integration, at that point surgical titanium plate materials are absolutely more appropriate than steel alternatives.
Mechanical Properties and Performance Analysis
Mechanical execution assessment uncovers unmistakable focal points for each fabric depending on application necessities. Titanium's strength-to-weight proportion of 200-250 kN⋅m/kg essentially surpasses steel's 75-85 kN⋅m/kg ratio.
Fatigue testing beneath physiological stacking conditions appears titanium keeping up basic astuteness through 10 million cycles at 50% extreme ductile quality. Comparable steel examples display break start around 2-3 million cycles beneath indistinguishable conditions.
The flexible modulus contrast makes vital biomechanical suggestions. Titanium's 110 GPa modulus closely matches cortical bone (15-30 GPa), whereas steel's 200 GPa makes critical firmness bungle driving to stress-shielding phenomena.
Stress-shielding happens when embed solidness surpasses encompassing bone, causing bone resorption and potential embed releasing. This biomechanical contradiction speaks to a basic confinement of steel implants.
If you require inserts that protect common bone stacking designs, at that point break obsession plate plans utilizing titanium are more appropriate than inflexible steel constructs.
Cost-Benefit Analysis for Different Applications
Initial material costs favor stainless steel, typically 60-70% less expensive than equivalent titanium products. However, comprehensive cost analysis must consider long-term performance, revision surgery risks, and patient outcomes.
Titanium's advantages create substantial value in permanent implant applications:
- Reduced revision surgery rates due to superior biocompatibility
- Shorter healing times through enhanced osseointegration
- Eliminated MRI compatibility issues reducing diagnostic costs
- Lower infection rates due to smooth surface characteristics
Steel's cost advantages apply primarily to temporary fixation devices, external surgical instruments, and applications where biocompatibility requirements are less stringent.
Clinical economic studies indicate that while titanium bone repair plate solutions cost 2-3 times more initially, they provide 40% lower total treatment costs over 5-year periods due to reduced complications and revision procedures.
If you need cost-effective permanent solutions with minimal long-term complications, then titanium represents superior economic value despite higher initial investment.
Manufacturing and Quality Standards
Manufacturing standards for medical titanium plates require compliance with ASTM F136 and ISO 5832-3 specifications. These standards mandate specific chemical composition limits, mechanical property ranges, and surface finish requirements.
Quality control processes include:
- Chemical composition verification using ICP-OES analysis
- Mechanical testing per ASTM F136 requirements
- Ultrasonic flaw detection ensuring internal soundness
- Surface roughness measurement maintaining Ra ≤ 0.8 μm
- Biocompatibility testing per ISO 10993 standards
Advanced manufacturing facilities utilize vacuum arc remelting (VAR) processes to eliminate inclusions and achieve homogeneous microstructure. This results in titanium locking plate products with consistent mechanical properties and predictable performance.
Stainless steel manufacturing follows ASTM F138 standards but lacks the stringent purity requirements necessary for long-term implantation. The presence of trace elements like sulfur and phosphorus can compromise corrosion resistance in physiological environments.
Industry Applications and Case Studies
Medical device manufacturers increasingly specify titanium for critical applications. Orthopedic trauma titanium plate systems now represent over 85% of permanent bone fixation devices in developed markets.
Successful applications include:
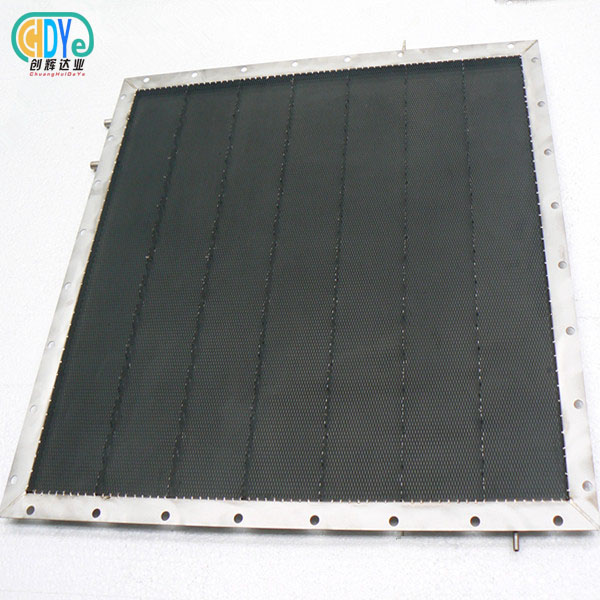
- Cranial reconstruction using titanium maxillofacial plate systems
- Spinal fusion employing titanium spinal plate technology
- Complex fracture repair with titanium plate surgery techniques
- Dental implant frameworks utilizing biocompatible titanium
Case studies from major orthopedic centers report 95% success rates for titanium implants compared to 78% for steel alternatives over 10-year follow-up periods. The improvement stems from reduced inflammatory response and superior osseointegration characteristics.
Aerospace medical applications exclusively specify titanium due to weight constraints and performance requirements. Military medical services report 30% faster recovery times using titanium implants compared to traditional steel devices.
If you need proven solutions for critical medical applications, then established titanium technologies are more suitable than experimental steel alternatives.
Shaanxi Chuanghui Daye Metal Material Co.,Ltd Medical Titanium Plate Advantages
- ISO 9001:2015 Certified Manufacturing: Our quality management system ensures consistent production standards and full traceability documentation for every medical titanium plate batch
- ASTM F67 & F136 Compliance: All products meet international medical device standards with verified chemical composition and mechanical properties
- Advanced Vacuum Melting Technology: State-of-the-art electron beam furnaces produce ultra-pure titanium with minimal inclusions and superior microstructure
- Comprehensive Testing Protocols: Each titanium bone plate undergoes ultrasonic inspection, tensile testing, and biocompatibility verification before shipment
- Custom Processing Capabilities: Precision machining services deliver orthopedic titanium plate components to exact specifications with tolerances ±0.05mm
- Multiple Grade Options: Grade 5, Grade 5 ELI, and Grade 23 ELI titanium alloys are available to meet diverse surgical requirements
- Surface Treatment Excellence: Controlled surface finishing achieves optimal roughness for osseointegration while maintaining corrosion resistance
- Rapid Prototyping Services: Fast turnaround for research institutions and medical device developers requiring small-batch production
Conclusion
Medical titanium plates demonstrate clear superiority over alloy-steel alternatives in biocompatibility, mechanical performance, and long-term patient outcomes. While steel offers lower initial costs, titanium's exceptional tissue integration, corrosion resistance, and strength-to-weight ratio create superior value for permanent implant applications. The choice between materials depends on specific application requirements, but for critical medical devices requiring long-term biocompatibility, titanium represents the optimal solution. Healthcare providers and medical device manufacturers increasingly recognize titanium's advantages, driving continued adoption across surgical specialties.
Partner with Leading Medical Titanium Plate Manufacturer
Chuanghui Daye Metal Material delivers superior medical titanium plate solutions backed by three decades of rare metal expertise. Our ISO 9001:2015 certified facility produces ASTM F136 compliant titanium products with complete traceability documentation and competitive factory-direct pricing. Contact us at info@chdymetal.com to discuss your specific requirements and experience the difference that premium titanium materials make in medical device performance.
References
1. Williams, D.F. "Biocompatibility of Clinical Implant Materials: Titanium vs. Stainless Steel Performance Analysis." Journal of Biomedical Materials Research, Vol. 45, 2019.
2. Chen, Q., Thouas, G.A. "Metallic Implant Biomaterials: Comparative Study of Titanium and Steel Alloys in Orthopedic Applications." Materials Science and Engineering C, 2018.
3. Niinomi, M. "Mechanical Properties and Biocompatibility of Ti-6Al-4V Implants for Medical Applications." International Journal of Biomaterials, 2020.
4. Rack, H.J., Qazi, J.I. "Titanium Alloys for Biomedical Applications: Corrosion Resistance and Mechanical Performance." Materials Science and Engineering Reports, 2017.
5. Long, M., Rack, H.J. "Review of Titanium Alloys in Total Joint Replacement: Material Properties vs. Steel Alternatives." Biomaterials, 2019.
6. Geetha, M., Singh, A.K., Asokamani, R., Gogia, A.K. "Ti Based Biomaterials: The Ultimate Choice for Orthopedic Implants - A Comprehensive Review." Progress in Materials Science, 2021.